Our 2021 Dallas/Fort Worth 3-Day Virtual Kick-Off started Saturday morning, November 7th, with an inspiring morning kick-off hosted on Zoom. The highlight was getting to hear Julie’s survivor story, which was both poignant and also made us laugh. If you missed it, here is Julie’s story, in her own words.
It is Monday January 7, 2019, about 3:30 p.m., and I am sitting at my desk at work when my cell phone rings. It is the doctor who performed a needle biopsy on my right breast three weeks ago. I have an appointment with her tomorrow, but she wanted to give me a heads-up that the biopsy results came back positive for breast cancer. For a moment everything around me ceased to exist, froze, and it is as if time stood still.
I was not surprised. Deep down I had known for some weeks, a couple of months even, that something was not right; that this time, this lump, was different. But I was still shocked. That may sound like a contradiction, but I know all of you will understand that narrow distinction between a feeling and facing the cold hard truth.
When my Susan G. Komen 3-Day coach, Tisho, asked me to speak at the Dallas/Fort Worth 3-Day Virtual Kick-Off I was a little hesitant, I felt that compared to so many others, my breast cancer journey was fairly uneventful, even easy. As I talked it through with my wife Dawn, she reminded me that my journey and story was not just about the discovery and treatment events of the past year and a half, but the three decades I spent “paying it forward”. I did this by fundraising for and participating in breast cancer awareness events, including two other 3-Days, and my strong belief in being an advocate for one’s own body.
I come from a female-centric family, yet none of us, female or male, had been diagnosed with breast cancer until my diagnosis last year. In spite of that, a number of us, myself included, have spent more than our fair share of time being squeezed by mammogram machines, lubed up for ultrasounds and needled for biopsies or had benign cysts drained.
So when I first noticed a lump in my right breast, mid-September 2018, I was not overly concerned. If anything, I was a little frustrated as I already had two mammograms in the past 10 months; one my routine annual and the other when a reoccurring cyst in my left breast got to the size that it was causing discomfort and required draining.
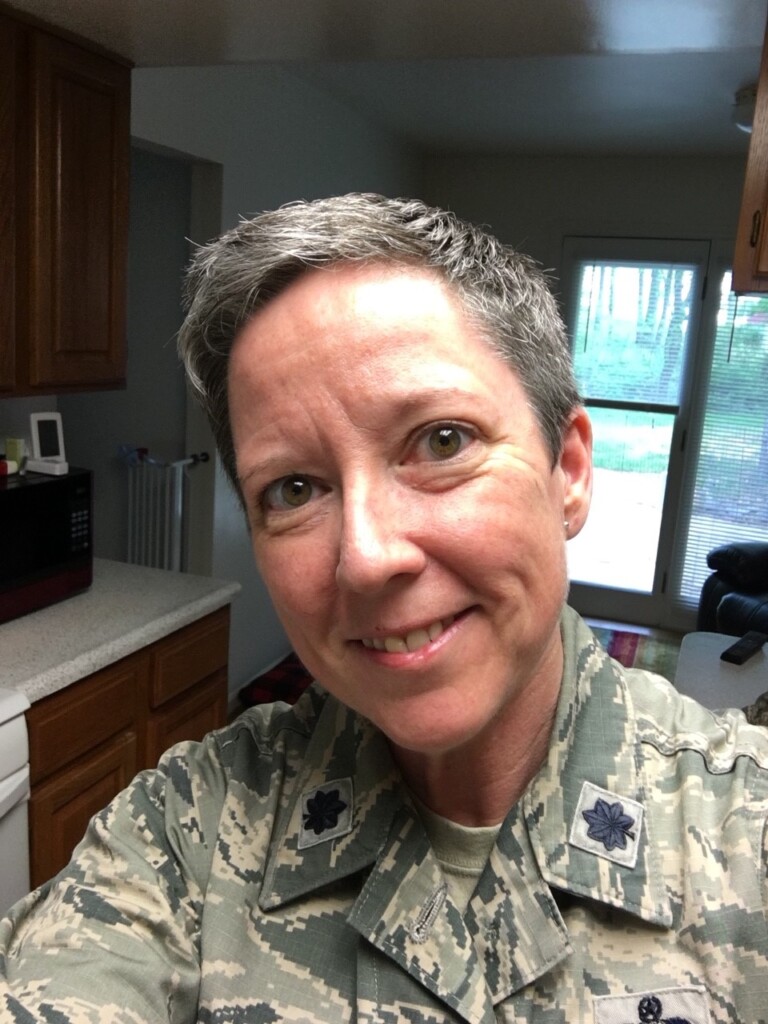
At the time I was still on Active Duty with the Air Force, I had recently moved to a new assignment and military base and was still getting settled at work and in my personal life, so I figured I would just keep an eye on the lump and try and “wait it out” until my next scheduled mammogram in a few months.
Then over the course of two weeks the lump grew noticeably and instead of feeling like the usual round tangibly unattached cysts, it became irregular and appeared to be connected to the breast tissue itself. At this point I realized my “wait it out” approach might not be the best way forward, so I went to the radiology department during their Walk-In hours to get checked out.
Well, it turns out you could only “Walk-In” if you just need an annual exam and have no symptoms. If like me you had a lump, you needed a referral from your primary care doctor for a scheduled appointment. Accomplishing those two steps took more than six weeks and it only happened that fast because I insisted on being a squeaky wheel. To say I was more than a little bewildered and frustrated would be an understatement.
By mid-October when I saw my primary care doctor, I was having noticeable discharge from my right nipple, enough that I needed to put a gauze pad in my bra each day. This was a first for me. Then there was how I was starting to feel physically in general. I do not even know quite how to describe it, I just felt “off’,” not myself. It was at this stage I started to think that something of significance could be going on.
The mammogram and ultrasound on November 19, 2018 showed exactly what I had been feeling, an irregular mass about two and a half centimeters long, made up of (according to the radiologist) a variety of different cell types, that while most likely benign (90% are) was worth further investigation by the Breast Care Center at Walter Reed Regional Medical Center in Bethesda, Maryland, as a precaution.
At this point I should say that I am what I like to call an optimistic realist. If the glass is nearly half full, I’ll call it half full, but if it’s only a third full, I’ll call it what it is. So, while I heard the radiologist’s words of optimism, somewhere deep inside I just knew I was going to be one of the other 10%. Over the next six months, I would become well acquainted with the amazing staff and facilities of the Breast Care Center, plastic surgery department, and oncology at Walter Reed Regional Medical Center.
The results of my December 16th biopsy revealed ductal carcinoma in situ. At this point, I should point out that my wife, Dawn, who I mentioned earlier, had only been my girlfriend for two weeks when I got my cancer diagnosis. But wow did she step up to help me get through both physically and emotionally. In addition, a week before my diagnosis, I had filed my formal retirement request after having spent over 27 years in the Air Force.
After discussing all the treatment options, recommendations and the fact that being the first in my family to be diagnosed with breast cancer technically put me at a genetically low risk for reoccurrence, I initially opted for a lumpectomy over a mastectomy. For “reassurance” it was decided to order a breast MRI just to confirm nothing else was going on.
So, on February 4, 2019, surgeons removed the mass, now four centimeters by two and a half centimeters and surrounding margins, and we all crossed our fingers and waited. While in the airport on Valentine’s Day waiting to fly from Washington, D.C. to Detroit to visit Dawn for a long weekend, my breast surgeon called to give me the news that results of tissue tests done along with my lumpectomy showed that they did not get clear margins. In other words, there were still some cancer cells left.
Also, the results of the MRI showed a few additional areas of potential concern. I do not know how most of you spent or envision spending your first Valentine’s Day with a new love but talking cancer treatment options is probably not at the top of your list. But that is what Dawn and I did that weekend along with talking to my parents and twin sister.
My mother at the age of 80 had gone through treatment for Stage 4 non-Hodgkin’s Lymphoma in 2018, the first known case of any type of cancer in my family, and so she more than anyone could understand what I was going through emotionally. As well as being a pretty optimistic person, I am also quite pragmatic, but there is something about knowing there is a living “thing,” a cancer inside you whose ultimate course if left unchecked would be to kill you, that is disconcerting even for the most rational of us.
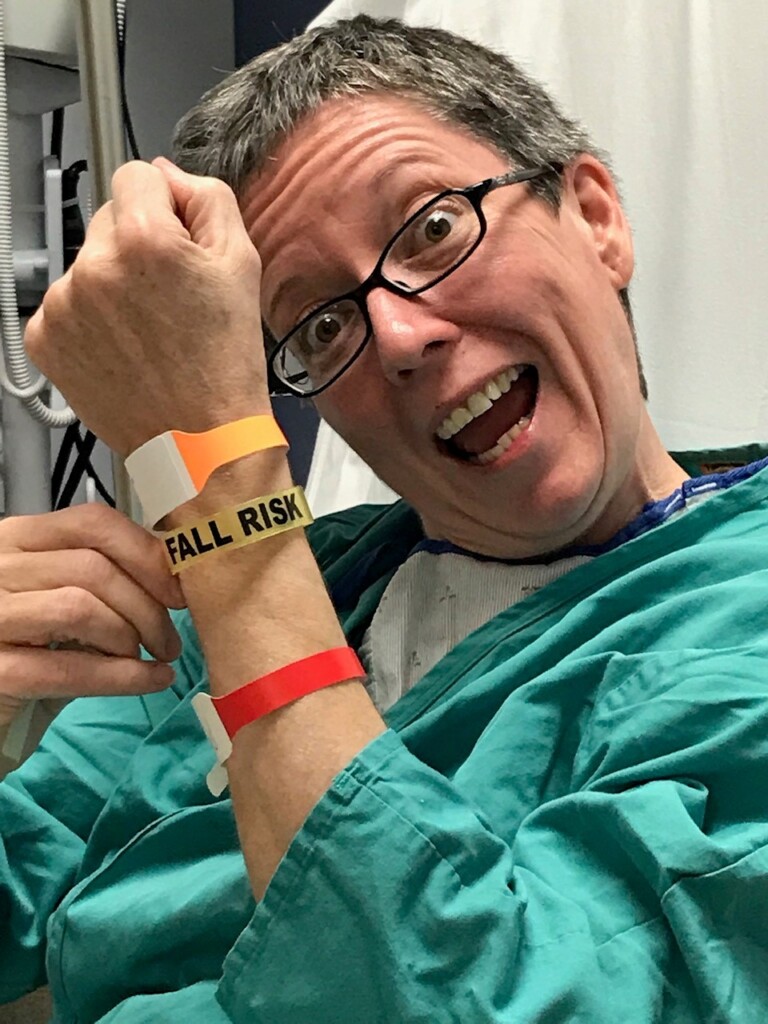
On March 11th, my right breast was removed during a skin preserving mastectomy. As at the time we did not know whether I would require radiation treatment, so a spacer was put in place until actual reconstruction could be scheduled. I had a nerve block prior to surgery and so the pain was minimal, but the fatigue and general loss of strength was unexpected.

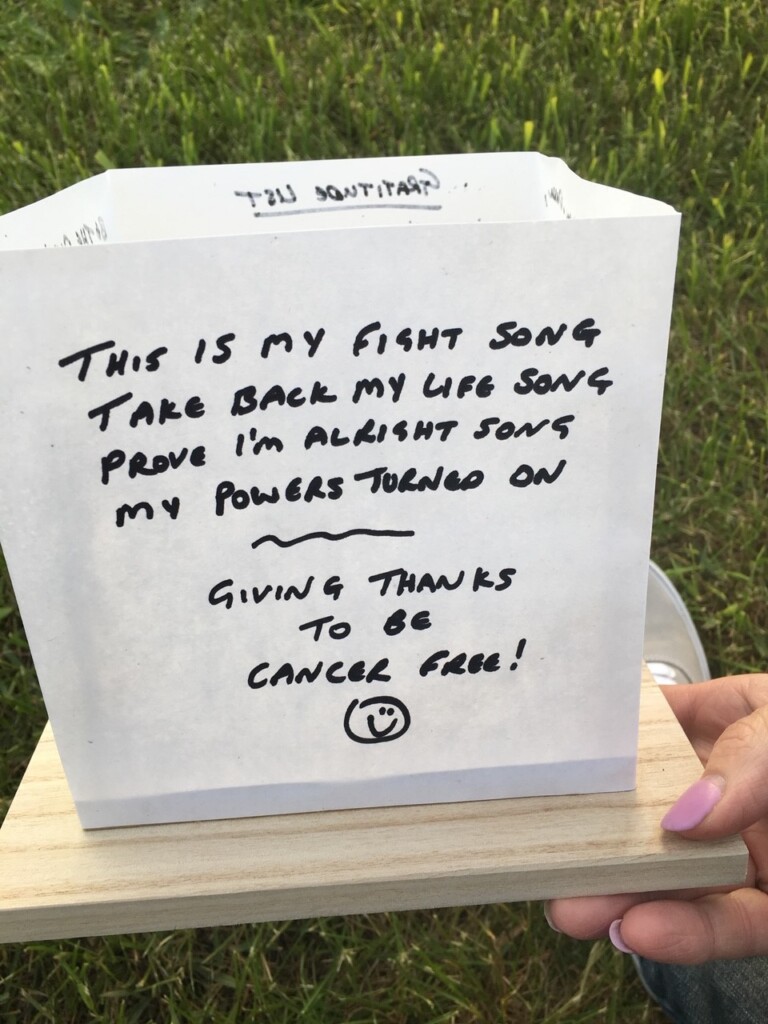
Dawn is a nurse and so after my initial follow-ups a week after surgery, we were permitted to go to Michigan for the rest of my convalescence and she was able to remove my remaining drain. Thankfully, tissue and lymph node testing results would show no trace of further cancer and so negated the need for radiation or chemotherapy. Having seen my mother go through chemotherapy, I was most concerned about having to do the same.
Reconstruction on the right breast via an implant and surgery to “lift” the left breast (so one side didn’t look like it belonged to a 20-year-old and the other to my 51-year-old body) were accomplished in May, and at that point, I honestly expected life would go back to normal.

Instead what followed were eight months of real struggle with the way my body now looked and felt and accompanying guilt over feeling that way, knowing that compared to many, I got off “easy” — no radiation or chemotherapy. I also struggled with my body’s reaction to taking the preventative hormone treatment Tamoxifen. I was having up to a dozen hot flashes a day. My sex drive and ability to enjoy physical intimacy all but disappeared. I was tired and getting depressed and I just felt disconnected much of the time.
In February of this year I made two decisions. One was to stop taking the Tamoxifen and schedule a prophylactic mastectomy on the left side. By then I had gotten used to how my right side looks and feels and taking all breast tissue out of the equation would address the nagging fear of a new episode of cancer occurring. And it would definitely help my wife Dawn, who would have preferred I had a double mastectomy to begin with. She’s more of a butt person than a breast person, so no loss there, LOL.
Then COVID-19 hit and the surgery had to be put on hold. It was finally rescheduled for the end of July, and then I got into poison oak while clearing land for a chicken coop and goat run and the surgery got postponed again. Is the third time a charm, or is the universe trying to tell me something? Well, I know the option to have the surgery is there for me when and if I want it.
One of the reasons I wanted to speak at the Kick-Off is to encourage you all to be ardent advocates for your own bodies and medical care. Listen to what your body is telling you and trust your instincts. If you do not get answers or care that makes you feel you are being adequately being taken care of, be the squeaky wheel. I was on the phone every day, sometimes multiple times a day, until I finally got a referral for a radiology appointment back in November 2018.
Experience is good, but sometimes youthful enthusiasm wins the day. A brand-new officer and doctor picked up my care and proactively got me in the queue for an appointment with the Breast Care Center while we waited on radiology. Once I was in the system at the Breast Care Center, my confidence level rose, and I would recommend them to anyone eligible to get care there.
In May of this year, Dawn and I moved from Michigan to Delaware into a house we had been renovating for the previous year. It sits on an acre and a half just outside of town and so we are realizing a lifelong dream of mine (and one Dawn has bought into) of a small homestead and pet-sitting business.

At this point I am feeling the full benefits of not taking the Tamoxifen and am under close surveillance by the Breast Care Center, so surgery is on the back burner for now. I think about giving the Tamoxifen another try, it might be the responsible thing to do. But I know I would not be able to stick with it if the side effects came back.
So for now the plan is to be diligent in keeping up with my follow-up plan and living life to its fullest, which brings me to the second choice I made in February of this year — to register for another Susan G. Komen 3-Day. When we walk in Dallas/Fort Worth next year, it will be 15 years since my first 3-Day and 12 years since I last walked.
I distinctly remember waiting in the finishing area of the 2006 Boston 3-Day, my first. As more and more finishers gathered, I commented to my friend on the palpable energy and that surely if there was anyone in there who was sick, there was healing power present. I can still feel it just thinking about it.
I have wondered what it will feel like participating next year as a survivor. I know I will feel immense gratitude. Gratitude for life, for sharing the experience with my wife (who will be participating for the first time) and gratitude for all the other participants (walkers and support staff and volunteers) present who are “paying it forward” until we find the cure.
We’re looking forward to seeing you in Dallas/Fort Worth in 2021, Julie and Dawn!
To hear more inspiring stories like this, you have one more chance by attending our San Diego 3-Day Virtual Kick-Off on November 21st. RSVP today.